Crossing the blood–brain barrier to deliver antibodies to treat Alzheimer’s disease – Innovation Toronto
Researchers led by Tokyo Medical and Dental University (TMDU) find that antibody fragments encapsulated in nanomicelles cross the blood–brain barrier and reduce the levels of toxic A? species in the brain of an Alzheimer’s disease model mouse
Sometimes the best things in life come by chance, when we happen to be in the right place at the right time. Now, researchers from Japan have found a way to ensure that new medications are delivered to the right place in the body and at the right timepoint in disease progression, so that they have the best effect.
In a study published recently in the Journal of Nanobiotechnology, researchers led by Tokyo Medical and Dental University (TMDU) have revealed that a novel delivery system delivers treatment to where it is needed most in a mouse model of Alzheimer’s disease (AD).
AD is a common neurodegenerative disease that causes dementia. It is characterized by the accumulation of a protein called amyloid ? (A?) in the brain, and a number of different toxic forms of A? have been identified that impair brain function, notably A? oligomers (A?Os).
“Multiple clinical trials have attempted to use an anti-A? antibody to treat AD, but the results have been unsatisfactory,” says lead author of the study Akiko Amano. “One potential explanation for this is that the blood–brain barrier (BBB) prevents most full-length antibodies from entering the brain.”
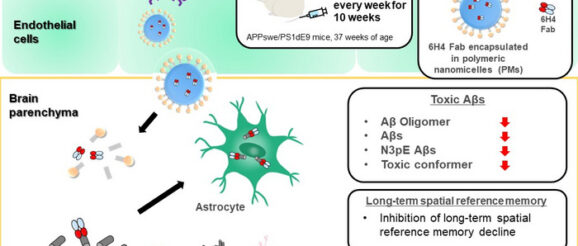
To address this challenge, the researchers previously developed glucosylated (sugar-linked) polymeric nanomicelles (PMs), which are tiny, hollow balls that could successfully cross the BBB via transcytosis in mouse brain capillary endothelial cells; this process was mediated by glucose-transporter-1 and induced by an increase in blood glucose levels after the mice experienced fasting conditions. In this study, Takanori Yokota and colleagues filled PMs with fragments of an anti-A?O antibody, injected them into a mouse model of AD, and assessed the effects on the brain and on behavior.
“The results were very clear,” explains senior author Nobuo Sanjo. “Administration of anti-A?O antibody fragments through PMs significantly reduced the amounts of various toxic A? species. In addition, the A? plaques that did form were smaller and less dense than those seen in untreated mice.”
Next, the researchers analyzed the behavior of the mice and found that the mice treated with the antibody fragment-filled PMs had better learning and spatial memory than untreated mice. “Our findings suggest that delivering sufficient levels of antibodies to the brain using PMs can reduce toxic A? species and slow AD progression in mice,” says Amano.
Given that the failure of anti-A? antibodies to improve cognitive function in human clinical trials was likely because of an insufficient supply of the antibodies in the brain, PM-encapsulated antibody fragments could represent an effective way to prevent AD progression. In addition, new candidates for AD treatment that degrade toxic A?s and reduce their toxic effects could also be delivered to the brain using the same PM-based system.
