Using ultrasound to treat pancreatic cancer effectively – Innovation Toronto
Sonodynamic immunotherapy proves effective in pancreatic cancer treatment
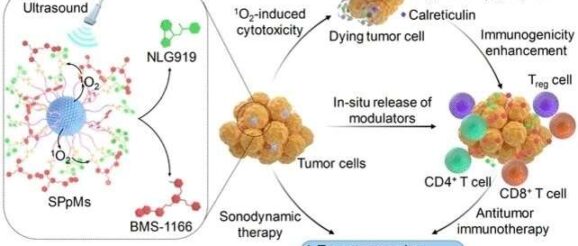
Ultrasound is a promising technique for treating cancer. Unlike laser light, used in photodynamic cancer therapy, ultrasound waves can reach deep into tissue—up to 12 cm—to treat deep tumors without damaging healthy cells. A team of researchers reporting in the journal Angewandte Chemie have now developed a sonodynamic cancer immunotherapy based on semiconducting polymer nanoparticles joined to immunomodulators that can be activated by ultrasound.
The principle behind cancer immunotherapy is using, or boosting, our own body’s defense mechanisms in the fight against cancer. However, this requires the tumor cells’ own defenses against our immune system’s T cells to be overcome. Although this can be achieved using special immunotherapeutic drugs, their action has to be limited to the cancer cells themselves to prevent an excessive and damaging response from the whole immune system.
In photodynamic therapy, activatable nanomedicines are transported into cancer cells on nanocarriers which accumulate in the cells and are then released by a reaction induced by laser light. However, laser light cannot reach the deeper parts of the human body, meaning photodynamic therapy is only of use for organs close to the surface and does not provide a solution for deep, difficult-to-treat cancers such as pancreatic cancer.
In contrast, ultrasound waves can penetrate into deeply located tissues with fewer side effects. Here, Kanyi Pu and a team of researchers from Nanyang Technological University in Singapore and Donghua University in China have used ultrasound for the first time for an effective sonodynamic treatment of orthotopic pancreatic cancer in a mouse model.
To make the sonodynamic immunomodulation molecular system, the team prepared nanoparticles from a specific semiconducting polymer that responds to ultrasound. Activated by ultrasound waves, it transferred its energy to molecular oxygen, from which singlet oxygen (a type of reactive oxygen species) was formed in the cells to induce immunogenic cell death and kill cancer cells. In addition, the polymer—or “semiconducting pro-nanomodulator”—carried two specific immunomodulators into the cells, which were released by singlet-oxygen-induced bond breakage after ultrasound activation.
The sonodynamic treatment was exceptionally effective in mouse models, with full recovery being achieved for mice implanted with orthotopic pancreatic tumors. Following injection into the bloodstream, the team used imaging methods to observe the accumulation of the nanomodulators in tumor tissue. Treatment with ultrasound then activated the drugs and the tumors broke down within a few days.
In other, healthy tissue, the nanomodulators that had not been activated were harmless. “However, immune-related adverse events were observed in the liver after the injection of the free drugs,” Pu says, acknowledging that the prodrug development is only at an early state. The team emphasizes that this sonodynamic method can be used to reach much deeper parts of the body than photodynamic therapy, hugely expanding the potential uses of immunotherapies that are activated at tumor sites.
