Microbiome-Based Health and Wellness Innovation: Reflecting on Regulatory Challenges and Needs | RAND
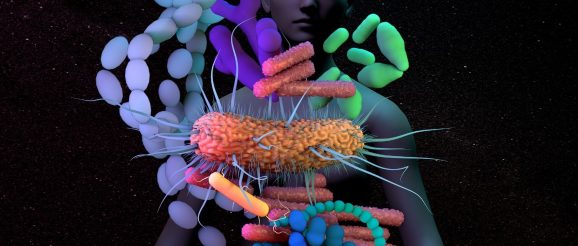
The microbiome, or the diversity of microorganisms that inhabit human bodies and that are estimated to make up half of people’s cells, is critical to human health. From enabling the work of the immune system to underpinning brain function, the microbiome has been linked to nearly every health condition. Health-related interventions seeking to manipulate the intestinal microbiome span diverse products such as drugs or therapies, foods and wellness products.
It’s hoped that Microbiome research and development may lead to an increasing number of therapeutic and well-being breakthroughs. And it’s estimated that the health-related microbiome market will reach up to USD 2.2 billion by 2025 (PDF). But regulating microbiota-related products poses a challenge that could require innovative approaches.
The regulatory approaches to microbiota-related innovations in the U.S., UK (PDF), and EU are generally based on product claims, which differ depending on whether products are classified as drugs or therapies, foods or wellness products.
For drugs and therapies, the pathway for approval is well-established and rooted in clinical trials focused on safety and efficacy, as regulated by agencies such as the US Food and Drug Administration (FDA), European Medicines Agency and the UK Medicines and Healthcare Products Regulatory Agency (MHRA) (PDF). This approach may yield differing results. For example, Faecal Microbiota Transplantation (FMT) for treating recurrent Clostridium difficile infection is approved by the MHRA (PDF) but not the FDA.
For foods that nourish and provide sustenance to the consumer (e.g. fermented foods such as yogurt that may have probiotic microorganisms) the pathway to approval faces less stringent criteria, based on general safety of consumption as regulated by the FDA, the UK Food Standards Agency, and European Food Safety Authority (EFSA). But although the pathway seems simpler for foods than drugs, it is not without challenges for manufacturers. Regulators can reject food manufacturer’s use of the probiotic label, given that this can be seen to imply a gut and immune health claim, akin to drug claims which would trigger a drug rather than food regulatory pathway. Supplements, functional foods (i.e., foods with added probiotics) and other wellness products require a regulatory pathway to approval that is similar for food.
The regulatory challenges also extend in part to the plurality of products in development and the nature of their claims, the state of microbiome science, the rapid pace at which innovation efforts are evolving, and the individualised nature of impact. Reflecting on key challenges in a timely manner is key to advancing regulatory agendas.
1. Classification clarity and its impact on regulation
The lack of clear criteria and standards on when to classify microbiome-based products as drugs and therapies, foods or wellness products can lead to confusion for innovators as to which regulatory pathways to follow. These challenges sometimes relate to a lack of clarity as to whether the claims associated with a product are health or wellness claims. The lack of clarity on product classification may also be a barrier to realising the full potential of a microbiome-based product, for example if innovators avoid making claims that would subject their products to lengthy drug regulatory pathways.
In addition, the same type of microbiome-based treatment can also be classified in different ways by different regulatory authorities. For instance, FMT is classified as a medicinal product in some geographies but as a biological product or tissue in others (PDF), leading to varied regulatory requirements.
2. Understanding appropriate evidence requirements and evidence generation processes
Evidence requirements for regulating microbiome-based innovations are also subject to some uncertainty. This is in part a reflection of the challenges of defining what constitutes a healthy microbiome, and the microbiome’s individualised nature (i.e. its variability between individuals, within individuals over time and its sensitivity to external factors like food and climate).
Understanding what constitutes sufficient evidence to determine the safety and/or efficacy of microbiome-based products is not straightforward.
Understanding what constitutes sufficient evidence to determine the safety and/or efficacy of microbiome-based products and to support patient access is not straightforward, given that these products can interact differently with individual microbiomes. It is therefore not surprising that probiotic health claims evaluated by regulatory bodies such as the EFSA, predominantly end up in the inconclusive territory of ‘possibly beneficial’. This personalised nature of impact of many microbiome-based products may pose difficulties to optimising trial designs, for example in terms of the number and nature of needed participants. In addition, the individualised nature of wellness (a claim for some non-drug products) may make it challenging to identify a set of universal wellness endpoints, especially if the same microbial agents may be beneficial for some people and harmful for others.
Innovative trial designs that can ensure a diversity of participants with different genotypic and phenotypic profiles and wider demographic considerations could have a role to play in regulatory innovation. For probiotics, some researchers have suggested a trial focus on the measurement of homeostasis (i.e. indicators of physiological equilibrium as endpoints in studies of health maintenance and wellness). Considering the balance of pre-approval evidence requirements and post-market real world surveillance may also be important for advancing regulation of microbiome-based products—both in terms of understanding benefits and monitoring potential adverse events over time. This may also matter given that the microbiome changes over time and is influenced by diverse external conditions which can impact on microbiome-based product functionality.
Similarly, there is relatively little evidence on how wider healthcare systems infrastructure (e.g. for manufacturing, storage, packaging, transport, distribution and administration, quality control standards) can impact microbiome-based product safety and/or effectiveness. Given how sensitive some of these products are to external conditions, it seems important to gather more evidence about appropriate handling methods that would inform guidance on safe and effective practices.
3. Regulating data access, sharing and use in microbiota-based innovation
A further challenge relates to issues around data ownership, access, sharing and use. There is a lack of clarity, for example, over whether bacterial strains taken from humans should be patentable and protected as intellectual property and with what degree of manipulation of the genome. There is also a need to advance the bioinformatic and physical infrastructure necessary to engage with biological samples and the personal data associated with it, safely and securely. Concerns about privacy and data sharing are not unique to microbiome-based innovation efforts, but the ease of potential access to microbiome-based data in matter containing personal microbiota accentuates regulatory challenges. For example, faecal matter consists of 95% micro-organisms, which in turn provides a potential plethora of personal information (such as a person’s environment and who they associate with).
In addition, microbiome studies often produce data with huge variability which can lead to many studies having inconsistent results—a data regulation infrastructure that can facilitate sharing of pre-competitive data and of methodological learning could help advance understandings of microbiome complexity and implications for health-related product development.
4. Appropriate communication with users of microbiota-based innovations
The increasing ‘popularity’ of microbiome-based products may make it important to engage in education and awareness-raising with the public and health practitioners about the state of evidence in the field, and the extent to which claims being made by some product developers are (or are not) supported by evidence. There has been an increased focus on transparent communication of evidence by regulatory agencies and innovators for some of the more controversial products (like probiotics), including through product labelling regulations. Further engagement and outreach are needed to understand information and evidence needs bottom-up, from the public directly as well as to manage any potential risks of misinformation.
Looking to the future
The pace at which microbiome science is advancing may need to be matched by the pace of regulatory innovation in the field.
The pace at which microbiome science is advancing may need to be matched by the pace of regulatory innovation in the field. This is a sociotechnical challenge that could require collaborative and coordinated action by regulators and engagement with wider stakeholders: innovators, healthcare professionals, the public and policymakers to ensure appropriate oversight and infrastructure, informed behaviours and effective innovation. Further research may be needed to determine where regulatory harmonisation may be possible and where variation is warranted. Clearer guidance for innovators on what constitutes health versus wellness claims also may be needed. Advancing thinking on what types of innovative trial designs and post-approval evidence collection can help accommodate the individualised nature of the microbiome also could merit attention. Timely research that can help prepare healthcare systems for future therapeutic developments may be equally important. For example, the microbiome challenges traditional understandings of health and disease and research could consider the implications of microbiome-based advances on training needs of healthcare professionals within clinical specialities outside of gastroenterology or infectious diseases and in terms of the organisation of patient care pathways. We hope that our reflections help inform a systematic approach to an innovative regulatory agenda by putting the spotlight on some of the key issues needing attention.
Mark Cabling and Zuzanna Marciniak-Nuqui are analysts in health and well-being at RAND Europe. Sonja Marjanovic is director of healthcare innovation, industry and policy at RAND Europe. The authors thank Nick Fahy for his helpful advice.
Commentary gives RAND researchers a platform to convey insights based on their professional expertise and often on their peer-reviewed research and analysis.
