Cancer Signals Hidden in Blood Now Visible with Dana-Farber Innovation | Dana-Farber Cancer Institute
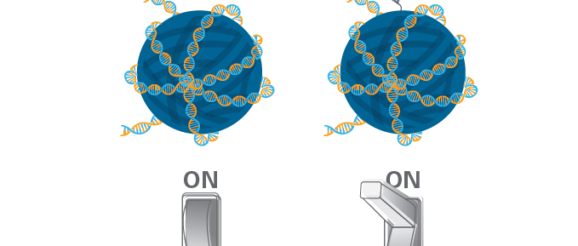
The same way you can predict whether a family is away, getting ready for work, or cooking dinner by observing which lights are on in the house, scientists can gaze into a cell and predict its state based on which genes are on or off.
Normal liver cells, for instance, have a predictable and recognizable set of genes switched on and off. But with the flick of a few switches, a liver cell can become cancerous. A few more switches can tip the cell into metastatic state.
DNA changes are not required to make such dramatic changes in the cell’s behavior. Rather, the switches can be envisioned as chemical tags that can be added or subtracted from histones, which are proteins that package DNA. These tags can either wind DNA more tightly, so the genes cannot be accessed, or loosen DNA, so genes become readily available for use. This collection of processes is called epigenetics.
Dana-Farber’s Matthew L. Freedman, MD, has spent the better part of the last decade cataloging the epigenetic signatures that occur in different types of cancer. To develop this body of knowledge, he and other researchers teased epigenetic signals out of cancer tissue from tumor biopsies.
But cancer tissue samples are hard to come by and slow to analyze, so Freedman and his colleagues developed technology to detect epigenetic signals of cancer in blood using a blood test, a “liquid biopsy”.
A Nature Medicine paper describes the results of their proof-of-concept study. The technology leverages lab techniques developed in Freedman’s lab, computational techniques from the lab of first author Sylvan C. Baca, MD, PhD, another Dana-Farber genitourinary oncologist, and the collaborative efforts of several Dana-Farber clinician-scientists including Toni Choueiri, MD, director of the Lank Center for Genitourinary Oncology at Dana-Farber, and a long-term close partner and collaborator of Freedman.
“This is the type of multi-pronged collaborations at Dana-Farber that result in meaningful novel discoveries and technologies,” says Choueiri.
“We’re excited about the potential for this blood-based technology to unlock new insights, because it allows us to do epigenomic profiling of cancer at a scale that was really unimaginable before,” adds Baca.
Epigenomic profiles in a milliliter of blood
The team’s blood test evaluates plasma from a single vial of a patient’s blood. Detecting clues about cancer in plasma is possible because the body is constantly shedding fragments of dead cells into the bloodstream. Those fragments include bits of DNA along with whatever epigenetic tags and structures were attached to them when the cell died.
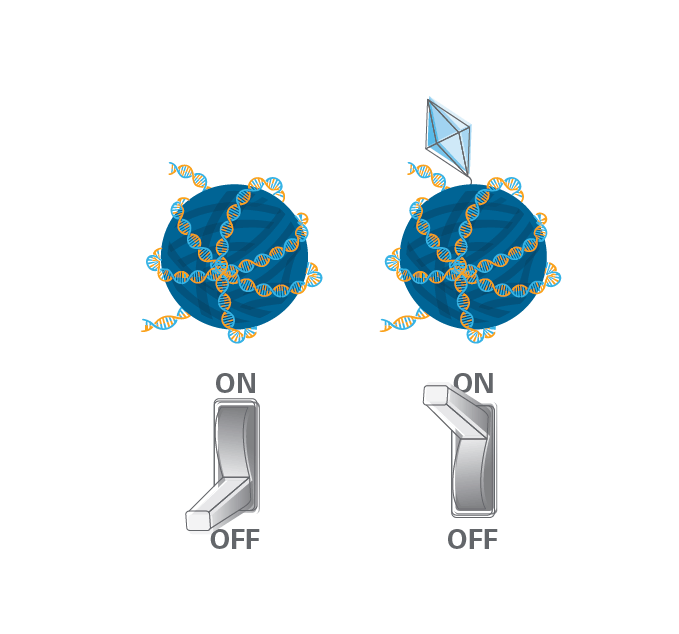
Freedman’s task was to pull the epigenetic fragments related to cancer out of plasma and leave the rest of the DNA behind. To do this, he used antibodies that recognize three specific epigenetic chemical tags.
There are many epigenetic chemical tags, but the three they targeted are known to flip genetic switches across the genome in cancer. As a result, the readouts of the test are called “epigenomic” profiles, because they provide a picture of these alterations across the genome.
The team sequenced the fragments of DNA attached to these epigenetic tags. DNA sequencing enabled them to determine which sections of the genome had been marked up — the equivalent of differentiating a light switch in the kitchen from a light switch in an office.
“The project involved a fair amount of both wet lab and computational innovation to get a very clear and high-quality signal,” says Baca.
The team wasn’t sure they’d be able to get a clear signal that was clear, but one night, after 7pm, Freedman walked into Choueiri’s office with results in hand, repeating “Can you believe this?”
Together, the information from this blood test forms an epigenomic readout of genes across the human genome that are switched on or off via epigenetic changes. That readout can reveal if the person has cancer and, if so, what kind, what drugs the cancer might respond to, if the cancer is resistant to a given drug, and more.
“When we saw that this could be done, we were over the moon,” says Freedman.
Validation in patients
To validate that the blood test results yield epigenomic profiles equivalent to those they’d catalogued from tumor tissue, they tested plasma samples from patients and compared the results.
The team evaluated the plasma of 433 patients who had been diagnosed with one of 15 types of cancer, almost all metastatic cases, as well as controls who had no cancer history. The team collaborated with clinicians at Dana-Farber, the National Institutes of Health, and Massachusetts General Hospital to obtain patient samples.
The epigenomic profiles they detected in these samples aligned with details about the cancer cases.
For example, in prostate cancer blood samples, the switches were on for the gene that encodes the protein PSA, which is typically elevated in prostate cancer cases. In patients with estrogen receptor-positive breast cancer, the switches were on for ESR1, a gene that encodes an estrogen receptor. They were even able to detect HER2-positive colorectal cancer, which is seen in only about 3% of cases, raising the possibility that the cancer might respond to available anti-HER2 therapies.
They also detected epigenetic activation of genetic programs typically turned on only during early development, when organs are forming rapidly, activation of tumor-driving genes called oncogenes, and silencing of tumor suppressor genes.
“We were able to do a fairly large-scale evaluation of how well this could capture epigenomic signatures of cancer,” says Baca. “This is a confirmation of the power of this technology across all 15 cancers we studied.”
Research continues
The team has a two-pronged strategy for the future. They have founded a company called Precede Biosciences that will focus on commercial development of the technology. But at Dana-Farber, the researchers will continue to study the potential for this technology to improve patient care.
In metastatic cancer, for example, there are many FDA approved drugs, but it often isn’t clear which one to choose for a patient. An epigenomic profile from a liquid biopsy could help doctors select the best treatment.
Epigenomic profiles from liquid biopsies could also be used to monitor patients during clinical trials to determine if the patient is developing resistance to their current medicine.
“Our collaboration with the clinicians here at Dana-Farber is essential if we want to make technology that is clinically valuable,” says Freedman. “If it’s not going to improve their clinical decision making and their ability to care for patients, then it’s a non-starter for us.”
