CFO’s guide to creating a successful innovation dashboard for healthcare
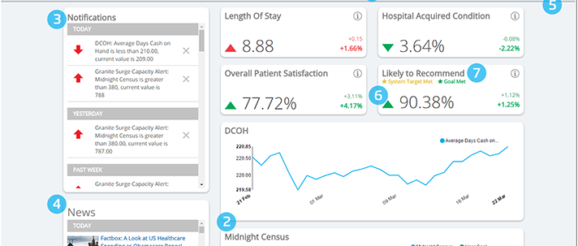
 Health Catalyst’s Leading Wisely dashboard
Health Catalyst’s Leading Wisely dashboard
At first blush, the concept of a hospital or health system having an innovation dashboard seems simple enough. And it is, in some respects. It’s a dashboard. It tracks innovative projects. There’s nothing opaque about the terminology.
Setting up a successful dashboard can be a multi-layered process, however, so it helps to have experience and expertise on your side. A good dashboard needs enthusiastic leadership, a technically sound framework, well-trained staff and good communication. Put those things together and you’re talking about a tool with the potential to boost business, big time.
Despite the moving pieces, the core of a dashboard is information, as systems track the development and efficacy of innovation projects within and without the organization. The data can be a lot to handle based on simple volume alone. A good dashboard is paramount, but all of the organizational pieces need to be in place before it can be leveraged effectively.
Duncan Gallagher has seen this firsthand. Gallagher is the recently retired chief financial officer of Allina Health, a $4 billion Minnesota health system.
“The key thing in getting a good one going is having energetic change- or achievement-oriented leadership that supports the change,” Gallagher said. “Without that, the dashboard is nothing more than a sheet of paper, or a graph on your PC, and if engagement is lacking the change isn’t going to follow.”
Once the leadership is in place, he said, the key next step is forming a focused and dedicated group to arrive at a consensus of what the organization is going to measure, but they’re going to measure it, and from what sources they’ll be pulling the data. It’s a long, lengthy step, but worth the time and effort.
At that point it’s time to look at the technical side of things. Do you want to use a table? Line graph? Bar graph? What’s the right visualization tool to convey performance?
“That’s the fun part,” Gallagher said. “You get to the design element.”
A good dashboard, in terms of both design and functionality, allows its users to decide how they want to communicate with the rest of the team. At that point, the tool becomes the critical communication point where process and accountability is concerned.
“It’s human nature to spend an inordinate amount of time deciding how and what to measure,” said Gallagher. “I can’t say there’s a requisite time. I think it’s a little bit of an art, and you need a strong leader to say ‘We have enough, let’s focus on the process change and start holding ourselves accountable for performance.'”
Michelle Cusack, chief financial officer of New York-based Northwell Health, said dashboards can be especially effective from a portfolio management standpoint.
“You want it to be a signal as to where you are with various aspects of the portfolio,” said Cusack. “With innovation, we look at where we are compared to where we had originally planned. We track it from a time perspective, and from a monetary perspective.”
Northwell’s dashboard is aligned with its due diligence: As a product goes through development, the system has real-time information coming back at them. For Northwell’s internal innovation, there’s an agreement of an objective, work plans, and an interdisciplinary team that’s driving the project, coupled with support from business units. Key milestones are developed as the process unfolds. Then comes execution, and figuring out the path to commercialization.
Determining key performance indicators and metrics
So which key performance indicators are necessary, anyway?
“Cash flow is always key — what we have as opposed to what we had anticipated in the plan,” said Cusack. “It’s as much the dashboard as the discipline to hold stakeholders accountable. The dashboard gets everyone on the same page, but it’s a disciplined approach to the team.”
Jay Spence, vice president of healthcare solutions a Kaufman Hall, agreed that revenue is important to track, and warned that too much information can be overwhelming; better to whittle it down to the essentials.
“I think the art of a good dashboard is not measuring 150 key indicators — because there’s probably 250 that organizations can report — but what are the most meaningful measures that are going to indicate our performance,” said Spence. “Cash on hand, cash to debt, capital expenditure as a percent of annual depreciation — those are the core financial measures that are the most important.”
Another thing that’s nice to have is context. Providing context in a dashboard via comparative measures is among the bells and whistles that Spence considers part of effective performance reporting and scorecarding. With it, you can compare your performance over time to that of your peers.
Monitoring operating cash flow margin, cash on hand and debt service coverage ratio certainly doesn’t hurt, either. And neither do clinical performance metrics.
“What we’re seeing more is an introduction of clinical performance measures, and putting those into our scorecard of financial risk,” said Spence. “The measures are starting to uncover where our clinical performance might have adverse effects on financial health.”
Beyond the numbers: accountability for innovative projects
As far as determining which processes a CFO should track, that picture becomes more challenging because of the transition to a value-based system.
“(Value-based care) doesn’t eliminate or even reduce the traditional measures of success under fee-for-service that a CFO needs to track,” Gallagher said. “They still need a handle on patient mix and days cash and productivity and length of stay, and those are very traditional fundamentals in fee-for-service. But they also need to track, under certain contracts, different metrics.”
Gallagher pointed to a need for the ability to drill down into a particular patient population, for instance, to understand metrics including utilization and cost per member, discharges per 10,000, and related changes.
According to Spence, the strategic goals of the business characterizes the direction in which organizations go with their dashboards and scorecards.
“The next evolution of that is, I need better context as to the broad work we’re doing as an organization every day,” said Spence. “A good scorecard will help evaluate, How are we performing today? Are we on track? If we’re not, it helps the organization to say, ‘Where do we want to focus our attention?'”
The shift to value continue to accelerate, which is good from a cost standpoint and good in terms of the availability of data. Performance on those contracts, though, has been one of the challenges for providers.
“They’re generally not able to get it as timely as the fee-for-service data, which makes sense,” said Gallagher. “Fee-for-service has been in place for 50 years or so, and the value-based structures have been evolving just over the past 10. Eventually it will be more readily available.”
Managing cost structures is also critically important when specifically tracking the implementations of innovative projects. The margin pressure on healthcare provider organizations is high, so they want to become more efficient and reduce costs.
“Beyond the numbers, it’s about who’s accountable, and are we on track to some of those targets as an organization,” said Spence. “The dashboard has often been charts and graphs and all about numbers, but it should also give visibility and transparency to, what are the initiatives we have going on today?”
That, he said, possibly has some cost-dollar savings attached to it. If an organization needs to reach cost reduction targets by, say, the third quarter, they need good visibility into what’s on track. It provides transparency to all that work.
Gallagher said innovative process changes and implementations need to be looked at almost as though the enterprise is managing a startup business.
“A lot of the health systems are very large,” said Gallagher, “$4 billion health systems that are used to how they operate, and the pace at which they operate, and these innovations tend to swim counter to those traditional processes, and may upend or dilute, or at least change, the decision-making and authority of different members in the value chain.”
Some of the more successful organizations have been able to set aside the people involved in innovation and let them run with the ball. But they have to be looking at key milestones for achievement with the innovations’ implementations with a higher sense of urgency than they do with some of the more traditional processes.
“One of the measuring sticks for me on that front is to what degree does the management team have on their agenda these transformative, innovative solutions, versus the traditional measures of success in fee-for-service, and how supportive they are of the transformational innovation initiatives,” said Gallagher.
As the team looks at those steps, Gallagher said dissonance will be created in the organization and will affect senior management members. What effect that has depends on whether management is tolerant of the dissonance, and whether they support and encourage it — or, if it breaches the senior management team, whether they decide to pause or terminate the innovation.
“When they underperform to a benchmark, it’s about whether they hold onto it and try to understand it,” said Gallagher.
Understanding there’s more than one type of innovation
Innovation can take many different forms.
Take Boston Children’s Hospital, for example. Boston Children’s was having a capacity management issue in the not-too-distant past, facing increasing demands for its services not only from a local and regional level, but also from sizeable numbers of national and international patients.
Because of this, Boston Children’s started a plan for building new venues, one that’s ongoing and slated t be completed within a few years. Long-term, that will ease demand. But they needed to do something now.
The hospital had to maximize its efficiency, using every bed and facility in its arsenal to its best effect. So it created a dashboard. A real-time, operational dashboard that enables staff to track the minute-to-minute status of its capacity, and future capacity.
That particular dashboard, dubbed Capacity Insight, rings together multiple data sources in a way that’s easy to handle. Senior leadership has access to it, of course, but so does the supervisor staff. Everyone has access, everyone is on board, and every right hand knows what every left hand is doing.
That’s critically important.
“Dashboards are being used as an ongoing management and feedback loop that’s getting created,” said Spence. “The data is ultimately a feedback loop. To the degree that the dashboard becomes a tool for measuring business performance, we know it’s an effective management tool.”
Detail is is a prime component of a successful dashboard, but how that detail is managed has a profound effect on its efficacy.
“It’s helpful to have some consistency for each of the projects, but detail,” said Cusack. “Originally we were focusing on the details project by project. It was too much to go through. The dashboard created transparency and accountability for the team. Having this document published and shared — it’s not something that stays in a group. It goes across the C-suite organization.”
As for whether the dashboard is working, well, from a CFO’s perspective that’s fairly easy to ascertain.
“Honestly, cash is king,” said Cusack. “It’s the key indicator. Once the projects are approved for a certain amount, it’s limited to that. The whole intent is to keep everyone up to speed on where we are.”
According to Gallagher, success with a dashboard occurs when the right measures and the right data are selected, and staff has done the appropriate planning around that. If you’ve shown improvement around the goal you’ve set, then by definition you’re having success.
“I suppose one could argue there could be some other downstream effects that are negative that the innovation impacts, but when you specifically link a process change with innovation … if you’re meeting the measure, then it’s working.”
A possible sign things aren’t going so well? At the board or mid-management level, if people walk through a set of dashboards or performance indicators and there are always one or two not meeting the mark, and it’s explained away in a facile manner … that’s a red flag.
“I always took that as a sign that we had given up on truly examining all of the barriers,” said Gallagher. “There was group-think of explaining it away. That was one way.
“The other was when I saw people try to modify the measures so they could change from red or yellow to green. The focus was on getting a green scorecard. Those are the big signs to me — whoever’s holding the leaders accountable for performance not accepting those answers, whether it’s at the board level, or senior management or mid-management, let’s not change the bar.”
How to know when your dashboard is working
Ask Spence and he’ll tell you that a successful dashboard has to drive corrective action within an organization. If it’s not doing that, it’s not an effective tool. The best dashboards are guiding and directing corrective action even if it’s more clinical in nature, such as trying to curb readmission rates. It makes those issues an organizational priority.
“From a financial performance reporting aspect, many times dashboards are used to compare history to history,” said Spence. “One of the things in healthcare is, I really need to look ahead. So dashboards provide that forward-looking view as well.
“In a financial sense, meeting financial goals is critically important, so forecasting … as part of the dashboard, that becomes actionable. That’s going to help me manage the dashboard more effectively. It brings my attention to things that need to be focused on, and I think dashboards that aren’t effective are always looking in the rearview mirror.”
Cusack is comfortable with where things are currently at Northwell. Describing the current moment as a “comfortable state,” she said there isn’t too much or too little information — though it will take diligence to ensure it stays that way. As with everything else, things in healthcare continue to evolve. Which is why it pays to be nimble.
Gallagher sees dashboards as critical to the future of healthcare, particularly with the fee-for-service system being gradually supplanted by value-based care. Dashboards can act as a North Star of sorts, guiding providers through the uncertain waters of change.
With the industry transitioning into an unpredictable future, it helps to have something constant, steady.
Focus on Innovation
In September, we take a deep dive into the cutting-edge development and disruption of healthcare innovation.
